In October 2024, after Vanderbilt Health notified an unspecified number of patients that they may have been exposed to HIV, hepatitis B and hepatitis C during endoscopy procedures, patients and healthcare workers across the country took notice. Many asked whether the current standard of care for endoscope decontamination, high-level disinfection (HLD), is adequate to ensure patient safety during endoscopic procedures.
The Crisis

Vanderbilt isn’t the only healthcare facility experiencing repercussions from infections linked to improperly decontaminated endoscopes. It is simply the latest to make the news.
In September 2013, the Centers for Disease Control (CDC) alerted the Food and Drug Administration (FDA) of multidrug-resistant organism infections (MDRO) and a possible association to procedures using duodenoscopes. In February 2015, the FDA acknowledged that duodenoscopes could remain persistently contaminated with life-threatening “superbugs” and related multidrug-resistant organisms.1,2 Examples of these potentially deadly microorganisms include carbapenem-resistant Enterobacteriaceae (CRE) and carbapenem-resistant Pseudomonas aeruginosa. In 2015, approximately 250 patient infections and 25 deaths were caused by CRE infections linked to improperly reprocessed duodenoscopes.
During its review of several duodenoscope-related outbreaks, the FDA found that many of the infections occurred despite “correct” cleaning and disinfection of the instruments in accordance with the manufacturer’s instructions. According to the FDA, “the complex physical design of duodenoscopes may impede effective reprocessing,”1 stressing that meticulously cleaning duodenoscopes prior to high-level disinfection (HLD) should reduce the risk of transmitting infection, but may not entirely eliminate it.”1
Previously, almost every infection associated with a contaminated duodenoscope or other type of flexible endoscope had been attributed to a reprocessing breach, more specifically, a failure to clean and disinfect the device as indicated in its labeling. Reprocessing a flexible endoscope as prescribed by the manufacturer had always been assumed to prevent cross-infection (with few exceptions) until the CRE transmissions in 2015.3
In August 2015, the FDA published a safety communication advising healthcare facilities to consider implementing one or more of four enhanced reprocessing measures, including low-temperature sterilization, to combat infection risk and improve the safety of duodenoscopes.2 Drawing a distinction between disinfection and sterilization, FDA stated that “duodenoscopes should be subjected to high-level disinfection following manual cleaning after each use. When possible and practical, duodenoscopes should be sterilized due to the greater margin of safety provided by sterilization.”2
Endoscope postmarket surveillance studies
After the 2015 outbreaks, the FDA required endoscope manufacturers to conduct field surveillance studies to sample reprocessed duodenoscopes in clinical settings to learn more about issues that contribute to contamination.
In May 2019, at the Healthcare Infection Control Practices Advisory Committee (HICPAC), FDA presented the results of the field surveillance study. Up to 3.6% of properly collected samples tested positive with low to moderate concern organisms. Up to 5.4% of properly collected samples tested positive for high-concern organisms, defined as organisms that are more often associated with disease, such as E. coli and Pseudomonas aeruginosa. The FDA also referenced studies indicating that repeated high-level disinfection cycles do not significantly impact the contamination rate compared to single HLD.
A Continuing Infection Risk?

Some data suggest that the incidence of a duodenoscope transmitting microorganisms, including CRE and other potentially deadly superbugs, during endoscopic retrograde cholangiopancreatography (ERCP), temporarily decreased following the FDA’s alerts in 2015 informing healthcare facilities and device manufacturers about the public health risk.
However, reports submitted to the FDA’s adverse event database for medical devices, or “MAUDE,” since 2015 indicate that, while the number of FDA reports linking a duodenoscope to an infection decreased in 2016 and even more so in 2017 compared to the relatively high number of cases reported to the FDA in 2015, the number of infections reported the next year, in 2018, reversed the trend, increasing significantly compared to the previous year (2017).
Additionally, the FDA received more than twice as many reports in 2019 linking a duodenoscope to infection or to device contamination (without necessarily an associated infection) compared to the previous year (2018), and almost three times as many compared to 2017.
The FDA stressed again in the 2020 alert that sterilization, particularly terminal (e.g., gas) sterilization, provides a greater margin of safety than high-level disinfection.”4
Bronchoscopes and urological endoscopes also pose a risk. In 2024, the FDA acknowledged that other types of flexible endoscopes also remain a concern and may pose a risk of infecting patients with superbugs and related multidrug-resistant organisms. In April 2024, FDA issued a letter to raise awareness among healthcare providers “about the risk of infections associated with reprocessed urological endoscopes, including cystoscopes, ureteroscopes, and cystourethroscopes.”5 These endoscopes are used for viewing and accessing the urinary tract. The FDA wrote this letter after acknowledging receipt of “numerous” medical device reports describing “patient infections post procedure or other possible contamination issues associated with reprocessing these devices.”5
Two months later in June 2024, FDA published a safety communication alerting the public to the risk of reprocessed bronchoscopes similarly infecting patients with multidrug-resistant bacteria, again including CRE.6 The FDA’s notice provides updated advice that supplements the FDA’s earlier (and now outdated) alert, published in September 2015, also discussing infections linked to reprocessed (flexible) bronchoscopes.7
This alert, focusing on bronchoscope, provided two new recommendations that were not discussed in the earlier 2015 communication: first, that healthcare facilities “consider using sterilization instead of high-level disinfection when feasible, because sterilization has a greater safety margin than high-level disinfection.” Otherwise, if “sterilization is not available,” then high-level disinfection of bronchoscopes should be performed.5
New Industry Guidance
As infectious outbreaks persisted, the healthcare industry received new guidance from the Association for the Advancement of Medical Instrumentation (AAMI). In 2021, the Technical Standards Committee released ST91:2021: flexible and semi-rigid endoscope processing in healthcare facilities. This document noted:
“Of greatest concern is the multiple and growing number of reports of multidrug-resistant organisms (MDRO) transmission resulting in patient infection and in some cases high rates of mortality.”
“Additional outbreaks have been reported related not only to duodenoscopes, but also to gastroscopes, ureteroscopes, cystoscopes, colonoscopes and bronchoscopes.”
“What is very concerning regarding outbreaks related to MDROs is that failures in the processing or the equipment could not always be identified. The facilities were following the guidelines and manufacturers’ written instructions for use (IFU).”5
AAMI ST91 2021 repeated FDA’s endorsement of the sterilization of flexible and semi-rigid endoscopes to be used in semi-critical applications whenever possible:
“Semi-critical devices which come in contact with mucous membranes or non-intact skin should be thoroughly cleaned and then sterilized. If sterilization is not possible, high-level disinfection is the minimum advised processing method. Historically, because of cost and logistic needs, the standard of care for gastroenterology and other endoscopes used in procedures performed outside of operating rooms has been high-level disinfection. It is advised that flexible and semi-rigid endoscopes to be used in semi-critical applications be sterilized prior to use. . . Sterilization of endoscopes can reduce this risk because of the greater margin of safety in the overkill process, and terminal sterilization provides a sterile packaged endoscope.”6
The Answer
Traditional low-temperature sterilization between 1960 and the 1990s required large amounts of ethylene oxide to achieve sterilization (10-6 SAL). Today’s modern-day sterilization requires far less EO per cycle. Medical instruments are sterilized in their final packaging, a process known as terminal sterilization, ensuring that instruments are completely free of viable microorganisms before use.
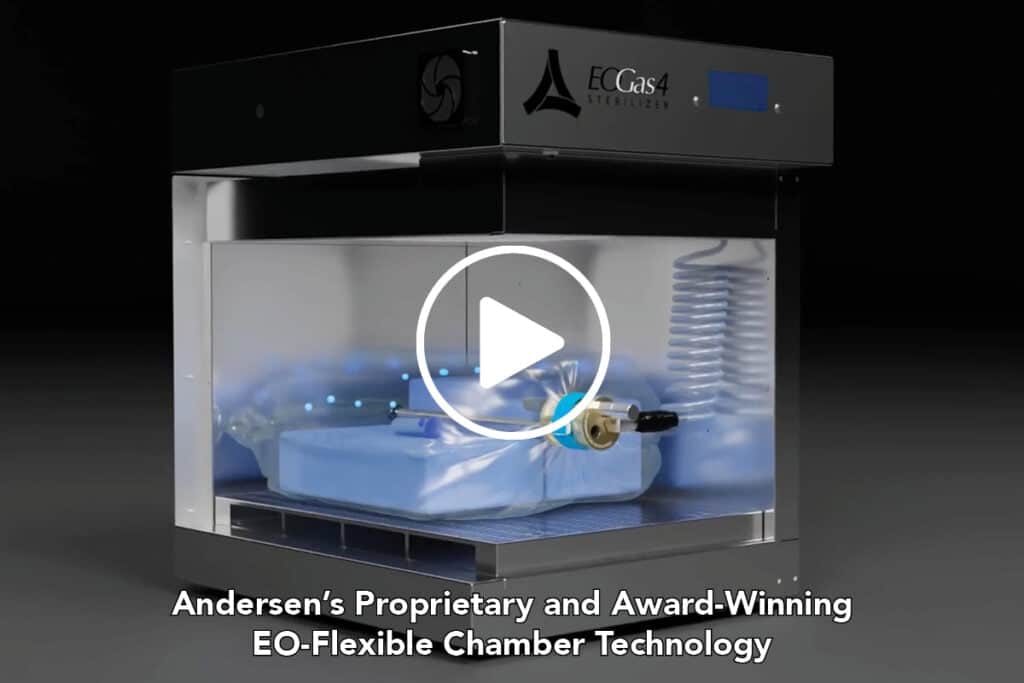
A. E. “Ted” May is president of Andersen Sterilizers, Inc., the leading manufacturer of FDA-cleared EO sterilizers, featuring award-winning EO-Flexible Chamber Technology® (EO-FCT). May also serves as co-chair of the Hospital Ethylene Oxide Working Group (WG62) of the Association for the Advancement of Medical Instrumentation (AAMI) Technical Standards Committee.
“Andersen Sterilizers recently released EOGas 4PLUS — the only system cleared by FDA for the terminal sterilization of all duodenoscopes and the longest colonoscopes on the market (≥ 1.2 mm ID, ≤ 3530 mm maximum length of any channel) while using the least amount of EO — just 17.6 grams per cycle,” shared May. “In 2019, Andersen was awarded the FDA Innovation Challenge 2 for reducing ethylene oxide emissions through our proprietary Ethylene Oxide-Flexible Chamber Technology.”
When ethylene oxide is paired with Andersen Sterilizers’ modern-day EO-FCT, only a fraction of the amount of gas, essentially a microdose, is needed to achieve terminal sterility. Sterilization and aeration take place in the same chamber within a dedicated cabinet requiring no external water or vacuum lines. Because excess air is removed from the flexible chamber, less gas is necessary. In contrast, gas sterilization modalities featuring a “rigid” chamber can require 10 times more ethylene oxide gas to reach the same level of terminal sterility.
The company was also recognized in 2020 by the National Steering Committee (NSC) of the Small Business Environmental Assistance Programs (SBEAPs) and Small Business Ombudsmen (SBO). Andersen received the
2020 Small Business Environmental Stewardship Award, an award recognizing small businesses that make significant contributions to protecting the environment.
“Environmental stewardship has been part of our DNA from the company’s founding,” said May. “As an American manufacturer whose medical devices are used all over the world, we are very proud to be recognized for our commitment to our technology and the environment.”
Andersen’s FDA-cleared sterilizers with Ethylene Oxide-Flexible Chamber Technology are the perfect complement to any infection prevention strategy as EO continues to be the only means for protecting the world’s immunocompromised patients from deadly microorganisms not eradicated by other modalities.
For more information on the Andersen Sterilizers EOGas 4PLUS and award-winning EO-Flexible Chamber Technology, visit sterility.com.
Footnotes
1 February 19,2015 “Design of Endoscopic Retrograde Cholangiopancreatography (ERCP) Duodenoscopes May Impede Effective Cleaning: FDA Safety Communication” https://www.lfm-hcs.com/alerts/FDA_duodeno_Feb_2015.pdf
2 August. 11, 2015 “Supplemental Measures to Enhance Duodenoscope Reprocessing: FDA Safety Communication” https://lfm-hcs.com/alerts/FDA_4_Supp_Mea sures.pdf3 February 4,2019
3 Feb. 4, 2019 “Use of Ethylene-Oxide Gas Sterilisation
to Terminate Multidrug-Resistant Bacterial Outbreaks
Linked to Duodenoscopes” https://bmjopengastro.bmj.com/content/bmjgast/6/1/e000282.full.pdf
4 January 17, 2020 “FDA recommends newer-designed duodenoscopes for better infection control safety” https://en.iacld.com/UpFiles/Documents/294330133.pdf
5 April 1, 2021“Infections Associated with Reprocessed Urological Endoscopes – Letter to Health Care Providers” https://www.LFM-HCS.com/FDA/FDALetterUrologyInfections2021.pdf
6 June 28, 2021 “Design of Endoscopic Retrograde Cholangiopancreatography (ERCP) Duodenoscopes May Impede Effective Cleaning: FDA Safety Communication” https://www.LFM-HCS.com/FDA/Safety2021Bronch.pdf
7 January 15, 2020 “FDA Press Release: The FDA is Recommending Transition to Duodenoscopes with Innovative Designs to Enhance Safety: FDA Safety Communication”https://www.einpresswire.com/article/507255538/the-fda-is-recommending-transition-to-duodenoscopes-with-innovative-designs-to-enhance-safety-fda-safety-communication
References & News Articles
Nashville Health Dept.: Some Vanderbilt patients may have been exposed to HIV, hepatitis (The Tennessean)
Naryzhny I, Silas D, Chi K. Impact of ethylene oxide gas sterilization of duodenoscopes after a carbapenem-resistant Enterobacteriaceaeoutbreak. Gastrointest Endosc. 2016 Aug;84(2):259-62. https://www.ncbi.nlm.nih.gov/pubmed/26855298
Bartles RL, Leggett JE, Hove S, Kashork CD, Wang L, Oethinger M, Baxter L, Brandabur JJ. A randomized trial of single versus double high-level disinfection of duodenoscopes and linear echoendoscopes using standard automated reprocessing. Gastrointest Endosc. 2018 Aug;88(2):306-313 https://www.ncbi.nlm.nih.gov/pubmed/29476847
August 8, 2023—Andersen Sterilizers & Andersen Scientific First Awardee in FDA’s 510(k) Ethylene Oxide Sterility Change Master File Pilot Program (Businesswire)
Feb. 19, 205 —Deadly CRE Germs Linked to Hard-to-Clean Medical Scopes (The New York Times)
March 18, 2015—Deadly bacteria outbreak inflames disinfection concerns (USA Today)
April 2, 2015—Duodenoscopes cause of E. coli outbreak in Washington (Healio)
August 5, 2015—Deadly infections from medical scopes go unreported, raising health risks (USA Today)
August 15, 2023—Andersen Sterilizers & Andersen Scientific First Awardee in FDA’s 510(k) Ethylene Oxide Sterility Change Master File Pilot Program