In dental practices, ensuring the sterility of dental instruments is essential to protect patients from infections and cross-contamination. While multiple sterilization methods exist, understanding what cold sterilization is and its applications for heat-sensitive dental tools can transform your infection control protocols. Traditional autoclaving poses significant risks to delicate instruments, making advanced low-temperature sterilization methods indispensable for modern dental practices.
When managing high-value, heat-sensitive dental devices, traditional autoclaving is not only impractical but also a liability. To protect your inventory from thermal degradation and ensure a rigorous 10⁻⁶ Sterility Assurance Level (SAL), you must understand what cold sterilization is. By utilizing non-thermal methods to disrupt microbial cellular structures, you achieve terminal sterilization for delicate polymers, fiber optics, and intricate handpieces that would otherwise fail under steam.
What is Cold Sterilization for Dental Instruments?
Cold sterilization represents a sophisticated advancement in terminal sterilization, enabling the achievement of a rigorous 10⁻⁶ Sterility Assurance Level without the destructive thermal stress associated with traditional autoclaving. This process utilizes chemical agents, specialized gases, or ionizing radiation to disrupt the molecular integrity of microorganisms while preserving the physical properties of even the most delicate materials.
Key characteristics of cold sterilization:
Non-thermal processing – Operates at ambient or low temperatures to prevent warping, melting, or material degradation
Chemical or gas-based agents – Use ethylene oxide (EO), hydrogen peroxide plasma, or other sterilants to neutralize pathogens
Deep penetration capability – Reaches complex geometries, narrow lumens, and internal channels that steam cannot access
Material compatibility—Suitable for heat-sensitive polymers, electronics, fiber optics, and delicate dental instruments
Terminal sterilization standard – Achieves 10⁻⁶ SAL, representing a one-in-a-million chance of a non-sterile unit
This non-thermal approach ensures that every surface and internal channel is rendered sterile, meeting the highest regulatory standards for patient safety in healthcare settings.
Methods for Dental Instrument Sterilization
Heat Sterilization (Autoclaving)
Heat sterilization involves subjecting instruments to high-pressure steam at specific temperatures and durations. While widely used, this method presents significant limitations for modern dental practices managing heat-sensitive equipment.
Advantages:
Highly effective in killing a wide range of microorganisms, including heat-resistant spores
Relatively quick process with efficient turnaround times
Compatible with basic metal instruments and heat-resistant plastics
Critical disadvantages:
Thermal degradation risk—Advanced dental instruments contain heat-sensitive polymers that warp or melt under autoclave temperatures.
Limited penetration – Steam cannot effectively reach narrow lumens or complex internal geometries.
Material compatibility issues—Fiber optics, electronics, and delicate handpieces cannot withstand high heat and moisture.
High operational costs—Requires significant maintenance, energy consumption, and infrastructure investment
Chemical Sterilization (Cold Sterilization with EO)
Chemical sterilization using ethylene oxide (EO) gas represents the gold standard for terminal sterilization of heat-sensitive dental instruments. This method eliminates microorganisms at low temperatures, making it ideal for instruments that cannot withstand autoclaving.
Ethylene oxide serves as the industry gold standard due to its exceptional material compatibility and deep penetrative capabilities. By operating at ambient temperatures, this process ensures that your most delicate instruments remain functional and safe for patient use.
Advantages of EO cold sterilization:
Superior material compatibility – Protects heat-sensitive polymers, fiber optics, and electronics from thermal damage
Deep penetration—Gas reaches narrow lumens, mated surfaces, and complex assemblies that steam cannot access.
Terminal sterilization standard – Achieves rigorous 10⁻⁶ Sterility Assurance Level (SAL)
Extended instrument lifecycle—Prevents thermal degradation, reducing long-term replacement costs
Versatile application—Suitable for complex-shaped instruments, small lumens, and porous materials
Considerations:
Requires specialized equipment and controlled conditions
Extended cycle times compared to autoclaving (includes aeration phase)
Must follow proper safety protocols for gas handling
Learn more about how Andersen’s sterilization process works to understand the complete cycle from loading to aeration.
Dry Heat Sterilization
Dry heat sterilization involves subjecting dental instruments to high temperatures in a moisture-free environment. This method suits instruments that may be damaged by steam but typically requires longer exposure times.
Advantages:
Eliminates moisture-related damage to instruments
Suitable for instruments sensitive to humidity
Disadvantages:
Longer exposure times are needed for effective sterilization (often 1-2 hours)
Still poses a thermal degradation risk for heat-sensitive materials
Higher equipment costs than autoclaves
Hydrogen Peroxide Plasma and Other Low-Temperature Methods
Newer technologies include hydrogen peroxide plasma sterilization and other low-temperature modalities. These methods offer alternatives for heat-sensitive instruments but come with specific limitations.
Advantages:
Lower operating temperatures than autoclaving
Shorter cycle times than traditional EO systems
No toxic residue concerns
Disadvantages:
Limited penetration capability for long, narrow lumens
Cannot sterilize cellulose-based materials or liquids
Higher per-cycle costs
To understand why ethylene oxide remains the preferred choice for complex dental instruments, consider the unique penetrative capabilities and material compatibility it offers.
Why Cold Sterilization is Essential for Heat-Sensitive Dental Tools
When you encounter devices with intricate electronics, fiber optics, or advanced polymers, traditional autoclave methods pose a significant risk of thermal degradation and structural failure.
Heat-sensitive dental instruments requiring cold sterilization:
Fiber optic handpieces – Contain delicate optical fibers that crack or degrade under high temperatures
Electric and battery-powered handpieces—House sensitive electronics vulnerable to heat and moisture damage
Dental implant instruments – Feature precision-machined components requiring dimensional stability
Endoscopes and intraoral cameras – Combine optics, electronics, and mechanical components
Plastic and composite-handled instruments—Made from polymers that warp, melt, or discolor under steam
Complex orthodontic tools—Contain mated surfaces and narrow channels where steam penetration is limited
Cold sterilization utilizes non-thermal agents to achieve a 10⁻⁶ Sterility Assurance Level without subjecting your valuable assets to the stress of high heat or moisture. By prioritizing low-temperature processing, you effectively extend the lifecycle of your most expensive dental equipment.
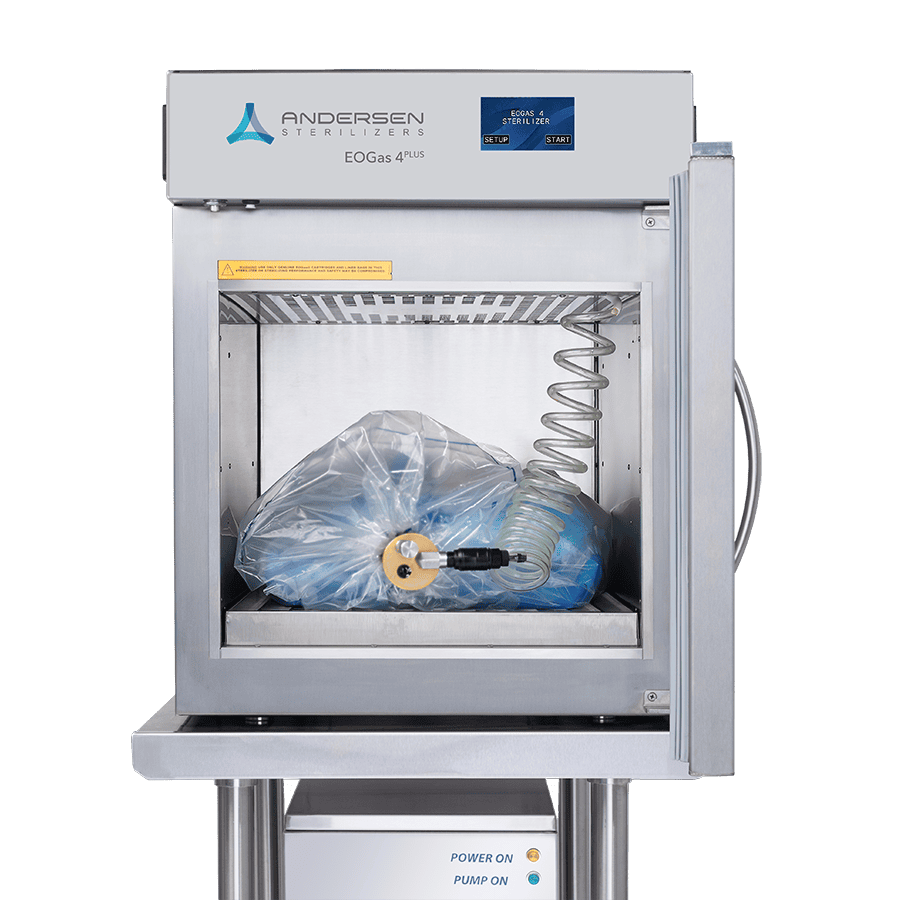
EO-Flexible Chamber Technology for Dental Practices
Proprietary EO-Flexible Chamber Technology optimizes gas consumption through a unique, vacuum-sealed delivery system that adapts to the specific volume of your load.
Key advantages of EO-Flexible Chamber Technology:
Optimized gas efficiency—Uses a fraction of the gas compared to traditional bulk sterilizers, significantly reducing operational costs
Reduced environmental emissions—Substantial reduction in EO released during aeration, creating a safer facility environment
Lower infrastructure requirements – Eliminates the high costs of industrial-sized abatement systems
Enhanced staff safety – Minimizes technician exposure through localized containment and controlled gas delivery
FDA-cleared reliability – Meets stringent regulatory standards for high-volume dental practice throughput
By concentrating the EO gas within a specialized liner bag, the system ensures deep penetration into complex geometries, such as narrow-lumen handpieces and multi-component dental kits. You can confidently process heat-sensitive polymers and delicate electronics without the risk of material degradation common with steam.
The versatility of this technology makes it an indispensable asset for sterilizing diverse inventories ranging from fiber optic handpieces to orthodontic instruments. You can manage the sterilization of moisture-sensitive instruments and complex procedure kits in-house with total control over cycle parameters.
Tools and Best Practices for Dental Instrument Sterilization
Ensuring the sterility of dental instruments requires specialized tools and adherence to validated protocols.
Critical sterilization tools:
Sterilization pouches and wraps—Medical-grade packaging that allows gas penetration while maintaining sterility post-cycle
Biological indicators – Validate sterilization efficacy by confirming complete microbial inactivation
Chemical indicators—Provide visual confirmation that instruments have been exposed to sterilization conditions
Ultrasonic cleaners—Remove debris and organic material before sterilization to ensure gas contact with all surfaces
Proper aeration equipment—Essential for removing residual EO gas, ensuring instruments are safe for immediate patient use
FDA-cleared technology provides you with a reliable solution that meets stringent regulatory requirements. The internal containment systems are engineered to prevent gas leakage, ensuring that your staff works in a secure atmosphere with minimal exposure risks.
Enhancing Dental Care with Advanced Sterilization Solutions
At Andersen Sterilizers, we specialize in offering advanced cold sterilization solutions for the dental industry. We ensure the highest standards of infection prevention through our comprehensive range of sterilization systems designed to maintain the integrity and functionality of delicate dental instruments.
Our systems guarantee complete sterilization with a Sterility Assurance Level (SAL) of 10⁻⁶, enabling your dental practice to deliver safe and effective care without concerns about germs or damage to heat-sensitive instruments. We support your dental practice with FDA-cleared technologies that are both user-friendly and cost-effective.
Protect Your Patients and Preserve Your Instruments
We provide gas sterilization solutions tailored to your specific dental practice requirements. Whether you’re managing a high-volume clinic or a specialized practice, we have the expertise and technology to ensure your instruments meet the highest sterility standards.
Contact our team to discuss how we can optimize your sterilization infrastructure and help you transition to advanced cold sterilization protocols that protect both your patients and your investment in quality dental equipment.
Frequently Asked Questions
What exactly is cold sterilization in a dental context?
Cold sterilization is a terminal sterilization process designed to achieve a 10⁻⁶ Sterility Assurance Level without utilizing destructive thermal stress. You utilize chemical agents or gaseous diffusion to disrupt microbial cellular structures, ensuring your heat-sensitive dental instruments remain pristine and patient-ready.
Why should I choose EO over traditional autoclaving for delicate dental instruments?
Traditional autoclaving poses a liability for high-value fiber optics, electronics, and advanced polymers due to thermal degradation and warping. By switching to EO cold sterilization, you maintain the physical integrity and functional longevity of your most sensitive devices while meeting the highest regulatory standards for safety.
How does EO-Flexible Chamber Technology improve operational efficiency?
Proprietary EO-Flexible Chamber Technology makes the sterilization process better by effectively killing germs while keeping emissions low and costs down. This FDA-cleared system allows you to process complex geometries and internal channels with unparalleled material compatibility.
Can cold sterilization guarantee the same safety levels as heat-based methods?
Yes, you can confidently achieve a rigorous 10⁻⁶ SAL through cold sterilization methods like EO gas diffusion. This modern method is a proven way to completely sterilize sensitive tools that can’t handle steam autoclaving.
Is EO sterilization environmentally responsible and safe for dental staff?
Advanced EO systems prioritize clinical safety and low emissions through sophisticated gas-phase methodology. You benefit from FDA-cleared technology that minimizes environmental impact while providing a reliable and cost-effective solution for your dental practice.
What dental instruments are best suited for cold sterilization techniques?
You should utilize cold sterilization for heat-sensitive handpieces, fiber optics, electronic instruments, delicate polymers, and intricate dental devices. These materials require the non-thermal processing provided by EO to avoid the catastrophic failure associated with high-pressure steam.
Spread the Word
Expert Guidance for Your Needs
Tell us about your sterilization requirements — our experts are here to guide you to the perfect EO solution.